Macular Diseases
Macular diseases can be treated and halted, and there is a possibility of restoring lost vision.
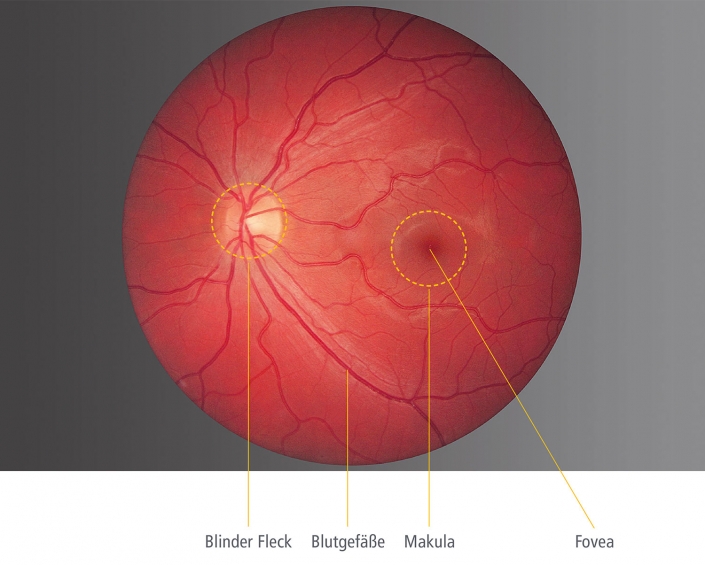
What is the macula?
The ‘macula lutea’ (yellow spot) refers to the center of the retina. This is the area where the retina has the highest resolution. Due to the high density of specialized light-sensitive cells, the macula enables us to recognize faces, read, and perceive color. Diseases of the macula therefore usually result in a significant deterioration of vision.”

Macular Degeneration
Macular degeneration is the third most common eye disease after cataracts and glaucoma. More than 4 million people in Germany are affected.
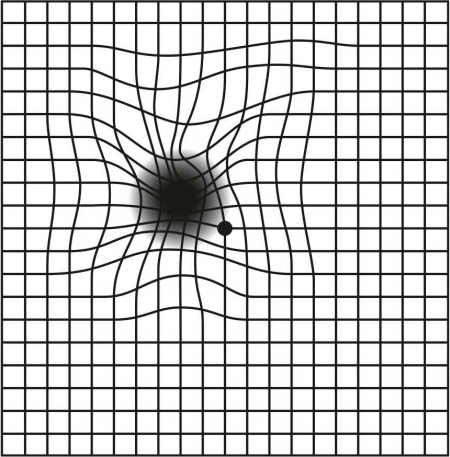
Those affected notice distortions and blurred vision in the center of their visual field.
Those affected notice distortions and blurred vision in the center of their visual field. Since the disease only affects the center of the retina, peripheral vision and spatial orientation are generally preserved, even in severe cases. The main cause of macular degeneration is aging of the central vision. Smoking and high blood pressure can cause macular degeneration to occur earlier. A family history is also observed in macular degeneration.
The ophthalmologist can detect signs of macular degeneration during a clinical examination, in which the center of the retina is examined using a special magnifying glass.
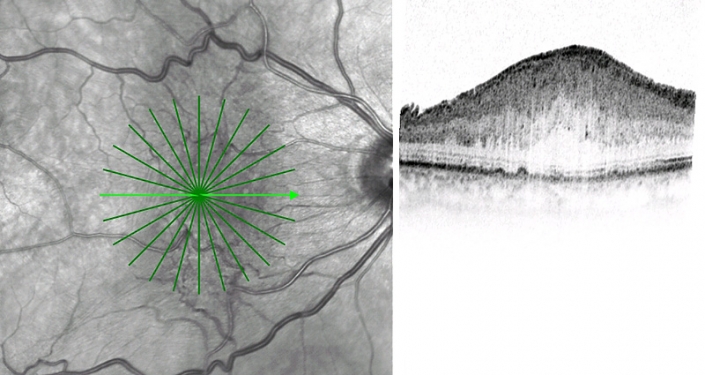
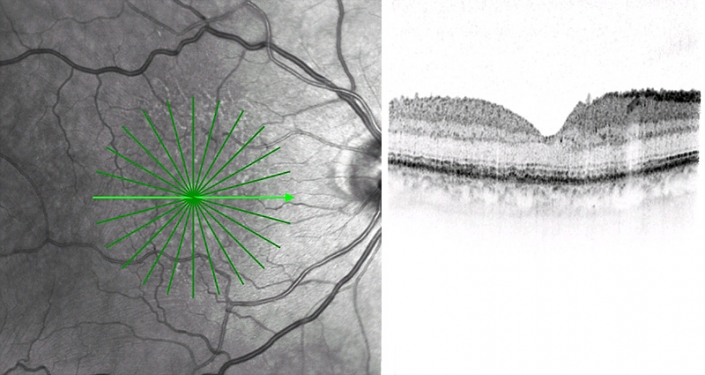
A more detailed diagnosis is possible with optical coherence tomography (OCT)
A more detailed diagnosis is possible with optical coherence tomography (OCT), which uses laser light to visualize the center of the retina down to the cellular level. The examination is non-invasive and is primarily used to monitor the progression of AMD.
Abnormal blood vessels, which can develop as part of AMD, are detected by a dye study (fluorescein angiography). During this examination, a special dye is injected into a vein in the arm and the vessels at the back of the eye are recorded with a special camera. The Regensburg Eye Clinic uses laser scanning angiography for better and gentler diagnosis instead of a conventional fundus camera. This examination requires less dye and allows for high-resolution and more detailed diagnostics.



Forms of Macular Degeneration
Two different forms of progression are distinguished in macular degeneration
Dry AMD
Nearly 90% of all affected individuals suffer from dry AMD. In this form of macular degeneration, the cell layer (retinal pigment epithelium), which nourishes the light-sensitive cells in the center of the retina, slowly degenerates. Visual acuity decreases over time, and central vision loss can occur.
Wet AMD
Although only 10% of cases are classified as “wet” AMD, it is responsible for 90% of severe vision loss associated with AMD. Wet AMD most often develops from dry AMD. Damage to the retinal pigment epithelium causes abnormal blood vessels to grow from the choroid into the retina. These fragile blood vessels lead to swelling of the central retina. Bleeding with scarring of the central vision can also occur. Wet macular degeneration typically progresses more rapidly than the dry form.
While wet macular degeneration cannot be cured, its progression can be slowed or halted. Treatment involves the use of special medications (VEGF inhibitors) that suppress the growth of abnormal blood vessels. These are injected into the vitreous cavity inside the eye using a fine needle under sterile conditions.
The Amsler Grid - Your First Self-Test for Retinal Disease
The Amsler grid test is a very helpful tool for detecting noticeable signs of retinal disease or for monitoring progress between medical treatments.
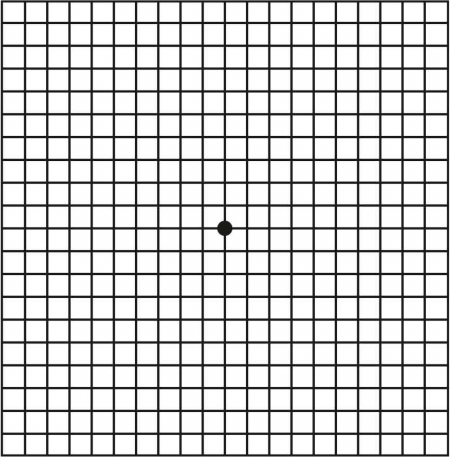

How to perform the Amsler grid test correctly:
Patients with cataracts often describe the following symptoms:
- If you wear glasses or contact lenses, please wear them during the test.
- Test each eye separately – cover one eye with your hand, for example.
- Hold the Amsler grid at reading distance (about 30 cm). Fixate on the black dot in the middle.
- Now assess how the lines around the black dot appear.
- Repeat the test with the other eye.
- Increased glare sensitivity while driving due to the headlights of oncoming vehicles.
If you see distorted, curved, or blurred lines, or if the lines appear interrupted or are missing altogether, you should see your eye doctor as soon as possible. Please mention the urgency when making the appointment!”
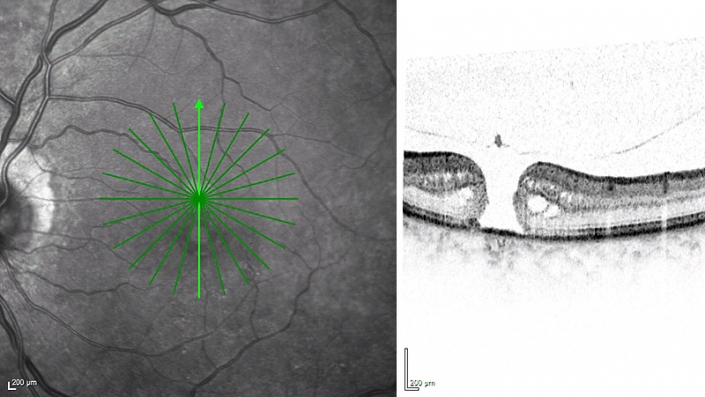
Epiretinal Gliosis or Macular Pucker
Epiretinal gliosis, also known as macular pucker, is caused by changes in the vitreous humor (the jelly-like substance that fills the inside of the eye). As the vitreous membrane separates from the center of the retina, it can lead to the formation of a fibrous tissue layer (gliosis) on the central vision area.
This gliosis is a thin membrane that forms over the macula, the central part of the retina responsible for sharp, central vision. As this membrane contracts and shrinks, it causes progressive wrinkling in the macula, leading to distortions (metamorphopsia) and a decrease in central visual acuity.
There is currently no medical treatment for epiretinal gliosis. However, the membrane can be removed through surgery (vitrectomy). Improvement in vision occurs gradually over the following months.
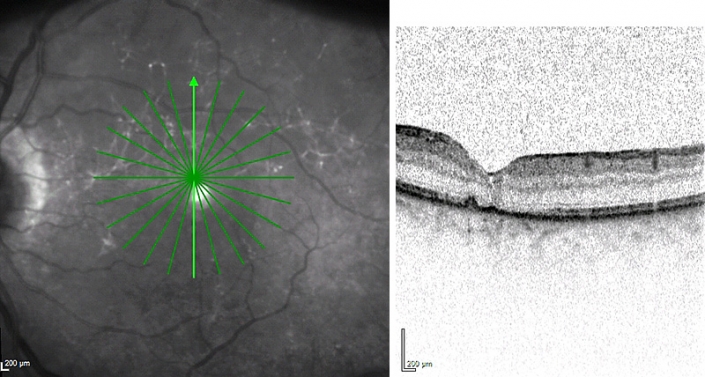
Macular Hole
A macular hole is a defect in the retina at the point of sharpest vision, the macula: Only in the visual center does the retina have a resolution that allows faces to be recognized and read.
Cause of a Macular Hole
The cause of a macular hole is, in most cases, traction on the center of the retina, triggered by degenerative changes in the vitreous humor. This transparent gel fills the eyeball and undergoes an age-related shrinkage process. Most patients affected are over 60 years old. Women are more likely to develop this condition than men. In up to 10% of patients, both eyes are affected over the course of their lives.
As with most macular diseases, patients initially report distorted vision, known as metamorphopsia. Later, patients notice a decrease in visual acuity or a blurred spot in the central visual field. If left untreated, in most cases the hole will grow larger, leading to further vision loss.
Larger Macular Holes
Larger macular holes can often be detected by an ophthalmologist during a clinical examination using a magnifying glass. A more detailed examination with a precise visualization of the defect is possible using optical coherence tomography (OCT).
Treatment of a macular hole is done through surgery. In a vitrectomy, the vitreous gel is removed through three tiny incisions of approximately 0.5 mm in diameter (23G or 25G). During the surgery, the traction on the center of the retina is relieved. These incisions typically seal on their own after surgery and do not require stitches. Afterward, a gas bubble is used to press the retina back into place.
A macular hole usually closes within a few weeks. Improvement in vision occurs slowly over the following months.
For very small holes, it is sometimes possible to relieve the vitreous traction with a special medication injected into the vitreous cavity, causing the hole to close.
Even if a macular hole has been present for a long time and vision is already significantly impaired, surgery can still improve vision.

