
Corneal collagen cross-linking
with riboflavin (vitamin B2) and UVA irradiation (crosslinking)
Cross-linking is a method for treating corneal diseases caused by insufficient corneal stability. These are collectively referred to as ‘ectatic corneal diseases’. The most common disease is keratoconus. Related corneal changes include keratoglobus, pellucid marginal degeneration (PMD), and post-LASIK corneal ectasia. These diseases lead to a conical protrusion of the cornea with a deterioration of visual acuity and quality.
Since 1988, collagen cross-linking has been used in ophthalmology and has been performed on many thousands of patients worldwide. The goal of treatment is to prevent further progression of the conical protrusion. Cross-linking cannot ‘cure’ the corneal disease.
The Therapy of collagen cross-linking
In the following, we would like to inform you about the therapy of collagen cross-linking. We would also be happy to provide you with more information about this innovative therapy during a consultation.
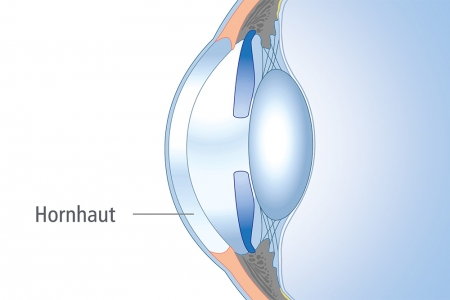
In all ectatic corneal diseases, the biomechanical stability of the cornea is reduced due to insufficient cross-linking of the corneal collagen.
The goal of cross-linking treatment is to increase the mechanical stability of the cornea by increasing the degree of collagen cross-linking in the cornea. To achieve this, vitamin B2 (riboflavin) is used as a photosensitizer and is illuminated with a UVA light source. This illumination triggers a photochemical process, resulting in the formation of new cross-links between the collagen fibers of the cornea, which increases the mechanical stability of the cornea. This prevents the progression of the conical protrusion of the cornea.
Cross-linking is performed on an outpatient basis. During the procedure, the eye is numbed with eye drops.
As a first step, the outermost cell layer of the cornea (epithelium) is gently removed to allow the riboflavin (vitamin B2) to penetrate the corneal tissue.
Then, the cornea is saturated with riboflavin by repeatedly applying riboflavin eye drops. This process takes approximately 30 minutes.
Afterwards, the cornea is illuminated with a UVA light source. By using a latest-generation UVA light source, as used in our clinic, the illumination time can be reduced from the original 30 minutes to now 10 minutes.
During the illumination of the cornea, the patient, lying on a couch on their back, fixates on a fixation light. Due to the use of anesthetic eye drops, the treatment itself is painless.
After the treatment, a soft bandage contact lens is placed on the cornea. This is left in place until the corneal surface heals. Additionally, patients receive an eye patch after the treatment, which they wear on the day of treatment and for the first night. This is to prevent accidental rubbing of the eye. The eye patch can be removed the day after the treatment or can be left in place until the visit to the ophthalmologist.
The goal of the treatment is to stabilize the cornea in order to slow down or, if possible, prevent the progression of corneal ectasia.
Therefore, the treatment should be considered when a progression of the ectatic corneal disease has been proven or is expected. Indications for a progression of the disease are frequent changes in contact lens or glasses prescriptions. A progression of corneal ectasia can be proven by repeated corneal topographic examinations.
Risk factors for rapid progression of corneal ectasia are an early onset of the disease or accompanying skin diseases (e.g., neurodermatitis, atopic eczema).
However, the treatment only makes sense if a usable visual acuity can still be achieved at the time of a possible treatment with contact lenses or glasses. Therefore, the treatment is all the more meaningful, the less advanced the deformation is
The corneal surface usually heals within three to five days after surgery. Initial pain or a foreign body sensation may occur. However, these symptoms can be alleviated with lubricating eye drops and pain medication. Immediately after the treatment, visual acuity is significantly worse than before. After healing of the corneal epithelium, visual acuity also improves significantly. Approximately 4 to 6 weeks after the treatment, the original visual acuity is usually restored.
Temporary side effects described include redness of the eye, itching, burning, blurred vision, and increased light sensitivity in the first few weeks after surgery. Additionally, almost all patients experience a gradually decreasing corneal haze for 3 to a maximum of 6 months, which can reduce contrast vision and night vision. In individual cases, hazes may remain permanently. However, the majority of patients do not find this bothersome. Serious complications, essentially a corneal infection or permanent corneal opacities in the form of scars and the associated deterioration of visual acuity, are very rare.
The cross-linking procedure has been performed in ophthalmology since 1988. In the meantime, many thousands of patients worldwide have been treated. In most cases, further progression of corneal changes could be prevented. In many cases, an improvement in findings has even been achieved in terms of a reduction in irregular corneal curvature. These effects can be observed at the earliest 3 months after treatment. Often, a decrease in corneal curvature can still occur up to 2 years after cross-linking. Since this cannot be predicted in individual cases, an improvement cannot be guaranteed.”
If you were already wearing rigid gas permeable (RGP) contact lenses before cross-linking, you can usually resume wearing them after four weeks. However, this should only be done after an eye examination to ensure that the contact lenses still fit properly. A new fitting of contact lenses is only advisable at the earliest 3 months after the procedure. Since the irregularity of the corneal surface can partially regress after the treatment, a repeated refitting of contact lenses may be necessary in the first few years after the treatment.
What aftercare is required following the treatment?
Eye drops and medications
To achieve optimal treatment results, it is necessary to apply eye drops regularly in the initial period after the treatment. A detailed dosing schedule will be provided after the treatment. Medications prescribed by your general practitioner can be continued on the day of treatment and in the following days without concern.
Pain and foreign body sensation
In the first 24 hours after cross-linking, increased tearing occurs. Swelling of the eyelids and redness of the eye are frequently observed. Not infrequently, patients report stinging pain, which in individual cases is described as very unpleasant. Pain-relieving medications and keeping the eye closed can alleviate these symptoms, although complete pain relief is often not achieved. In the first few weeks, many patients describe a foreign body sensation, which can be alleviated by the use of artificial tears.
Follow-up appointment with the eye doctor
After the treatment, we recommend regular eye examinations until the corneal surface has completely healed and the bandage contact lens has been removed. When and how often follow-up examinations are necessary depends on the healing process. These check-ups are absolutely necessary for the early detection of any possible complications (such as an infection).
Physical activity/sports
You should take it easy for the first few days after the treatment. This is especially true for physically demanding sports and activities where there is a risk of infection from sweat coming into contact with the eye. You should avoid dirty environments for the first few days.”
Driving
Whether and when you can drive again after the surgery depends on your visual acuity after the treatment and the visual acuity of your other eye. Your eye doctor will discuss when you can resume driving after the cross-linking procedure.
Reading, computer work, watching TV
These activities will not harm your eyes after the treatment. However, as they can cause your eyes to dry out more, you should regularly use artificial tears to moisten your eyes.
Work/school
When you can return to work after the treatment depends on your job. Generally, you can fully resume your work after only a few days, provided the visual acuity of the treated eye or both eyes together is sufficient for your job. Attending school is also usually possible again after a few days.
If you experience a worsening of your eye condition after treatment (e.g., severe redness and crusting of the eye, pain, vision loss), you should immediately contact your treating ophthalmologist or the ophthalmic emergency service.

