Retinopathy and Maculopathy
What is a diabetic eye disease?
Diabetes is a systemic disease that affects all parts of the body. The specialists at the Eye Clinic Regensburg focus on treating the changes that diabetes causes in the eye.
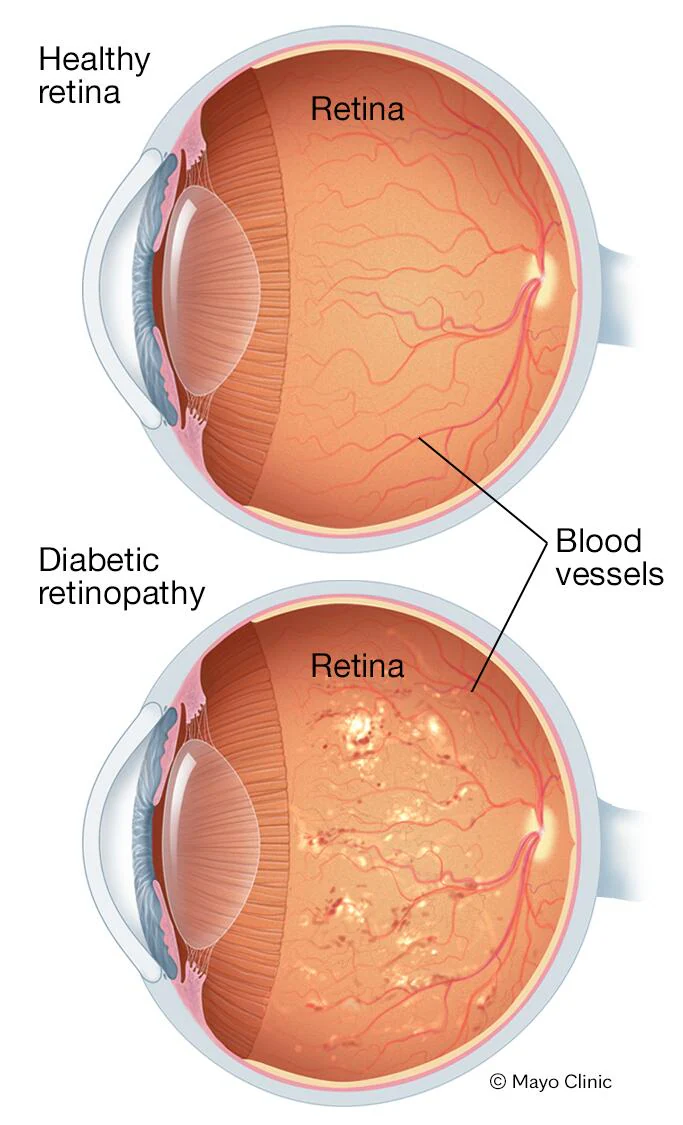
Diabetic retinopathy is a disease that attacks the walls of the smaller blood vessels in the eye, leading to sac-like bulges in the vessels. This can result in leaks and bleeding in the eye. Without treatment, insufficient oxygen supply to the eye can lead to the growth of abnormal blood vessels and ultimately blindness.
Uncontrolled blood sugar levels can cause visual disturbances such as diabetic macular edema, advanced diabetic eye complications, and cataracts.
Symptoms are not always noticeable, but blurred or distorted central vision, sudden appearance of spots in the visual field, or visual field defects in diabetics must be examined as soon as possible.
We recommend that you have your eyes examined regularly, even if you do not have any vision changes. This is because diabetes can gradually impair your vision, and if diabetic retinopathy is too advanced, it may not be successfully treated.
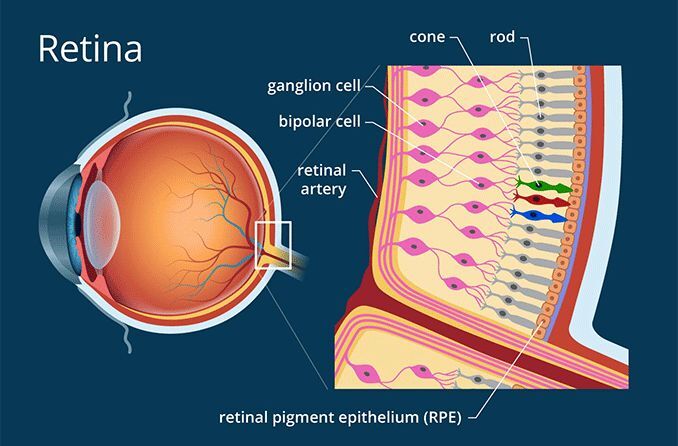
What is the retina and how does it work?
The retina is a thin layer of tissue that lines the inside of the back of the eye.
The retina is supplied with oxygen and nutrients by blood vessels. Light enters the eye through the front part (cornea, pupil, and lens) and is focused on the retina.
Simply put, the retina can be divided into two main parts: the macula, which is responsible for our sharp and detailed central vision, and the middle and peripheral retina, which is responsible for our peripheral (side) vision and helps us detect movement.
The retina converts light into electrical signals, which are then sent to the brain.
Who can get diabetic retinopathy, and what should be considered?
All patients with diabetes are at risk of developing diabetic retinopathy. The longer you have diabetes, the greater the risk.
What can you do to protect your eyes from diabetic changes?
You can reduce your risk of developing severe diabetic retinopathy by attending your regular diabetic eye exams. If necessary, additional OCT scans of the central retina and ultra-widefield images of your retina can complement the clinical examination. At the Eye Clinic Regensburg, we specialize in screening for and treating diabetic retinopathy, and we would be happy to schedule an appointment for you.
- Keep your blood sugar (HbA1c), blood pressure, and cholesterol levels within the target ranges agreed upon with your diabetologist (endocrinologist) and general practitioner.
- Exercise regularly, stay active, and eat a healthy diet.
- If you smoke, try to cut down or quit smoking. Reduce your alcohol consumption.
What does diabetic retinopathy look like?
Non-proliferative diabetic retinopathy
Non-proliferative retinopathy refers to the early stages of diabetic retinopathy.
Tiny, red dots called microaneurysms develop in the blood vessels. Larger hemorrhages within the retina may also occur.
Non-proliferative retinopathy typically does not affect vision and may not require immediate treatment. However, regular monitoring is essential, and your diabetes should be managed as closely as possible by your general practitioner or diabetologist. The frequency of follow-up examinations is determined individually based on the severity of the changes. Over time, the blood vessels may narrow, leading to insufficient oxygen and nutrient supply to the retina. Without treatment, this progression can result in proliferative retinopathy and blindness.
Proliferative diabetic retinopathy
This stage follows non-proliferative retinopathy. In this stage, abnormal, new, and fragile blood vessels can develop. These new blood vessels may not initially cause symptoms or vision loss. However, your vision is already at risk because the new vessels can bleed or form scar tissue that can pull the retina away from the underlying layers of the eye (retinal detachment). These complications may require vitrectomy and targeted laser treatment to stabilize or improve vision and prevent blindness. Fundus fluorescein angiography helps to visualize leaky new blood vessels caused by proliferative retinopathy.
What does diabetic retinopathy look like?
Non-proliferative diabetic retinopathy
Non-proliferative diabetic retinopathy refers to the early stages of diabetic retinopathy.
Small changes occur in the blood vessels, which appear as tiny red dots, called microaneurysms. Larger red spots may also occur, which are due to bleeding within the retina.
Non-proliferative retinopathy usually does not affect vision and may not require treatment. However, it is important to monitor the condition and to ensure that your diabetes is managed as well as possible by your general practitioner or diabetologist. The appropriate interval for check-ups will be determined individually depending on the severity of the changes. Over time, the blood vessels may narrow, and the retina becomes undersupplied with oxygen and nutrients. This progression can lead to proliferative retinopathy and blindness if left untreated.
Proliferative diabetic retinopathy
This stage follows non-proliferative retinopathy. In this phase, abnormal, new, and fragile blood vessels can develop.
These new blood vessels may not cause any symptoms or vision loss on their own. However, at this stage, your vision is already at risk because the new vessels can bleed or form scar tissue that can pull the retina away from the underlying layers of the eye (retinal detachment). These complications may require a vitrectomy and targeted laser treatment to stabilize or improve vision and prevent blindness.
Fundus fluorescein angiography helps to visualize leaky new blood vessels caused by proliferative retinopathy.

Diabetic maculopathy
In diabetic maculopathy, central vision is impaired. Reading small print, recognizing fine details or faces, and distinguishing colors can become difficult.
This is usually caused by fluid, fats, and proteins leaking from small blood vessels into the macula. The swelling that accompanies this leakage is called edema. Intraocular injections such as anti-VEGF injections or steroid implants can be used to prevent further vision loss and even improve it in some patients.
If the blood vessels in the macula narrow too much, no oxygen can flow to the retina and the tissue "starves." This causes the cells that capture light to die and vision to deteriorate.
The term for this condition is "ischemic maculopathy." Currently, there is no treatment for ischemic maculopathy.
Prevention through optimal control of your diabetes and other blood parameters such as blood pressure is essential here as well.
How can I tell if I have diabetic retinopathy or maculopathy?
Diabetic retinopathy and maculopathy can occur individually or in combination.
Initially, neither condition causes any visual symptoms. Even stages requiring treatment may not produce any visual symptoms in some patients.
Diabetic retinopathy and maculopathy are detected through an annual examination of the fundus (retina) with fully dilated pupils. In some cases, a non-invasive retinal examination using OCT scans is necessary.
Innovative technologies such as ultra-widefield imaging, which allows visualization of a significantly larger area of the retina compared to standard photography, as well as optical coherence tomography and angiography, can enable earlier diagnosis.
Treatment of diabetic retinopathy and maculopathy
If you develop proliferative diabetic retinopathy (the growth of abnormal, new blood vessels) or maculopathy, you will be recommended for examinations and treatments.
The goal of treatment for proliferative diabetic retinopathy is to prevent the formation of new abnormal blood vessels in the retina. If treatment is successful, the new vessels will shrink, and some of them will even disappear over the course of a few months.
The goal of treatment for diabetic maculopathy is to reduce swelling or edema. Treatment is tailored to the stage of the disease and the patient and may include one or more of the following measures: anti-VEGF or steroid injections, laser treatments, or a vitrectomy.
Laser treatment can be applied either to a localized area or to the entire retina, excluding the macula, or to both.
If you develop high eye pressure or glaucoma, drops may be administered to control the pressure and reduce the risk of long-term damage.
If you develop a cataract as a result of diabetes, surgery is necessary to remove the cloudy lens in your eye, which is then replaced with a clear artificial lens implant (intraocular lens).
If you develop a vitreous hemorrhage or scar tissue that causes a retinal detachment, a vitrectomy may be necessary.

