
What is a Macular Hole?
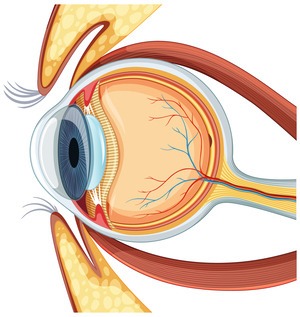
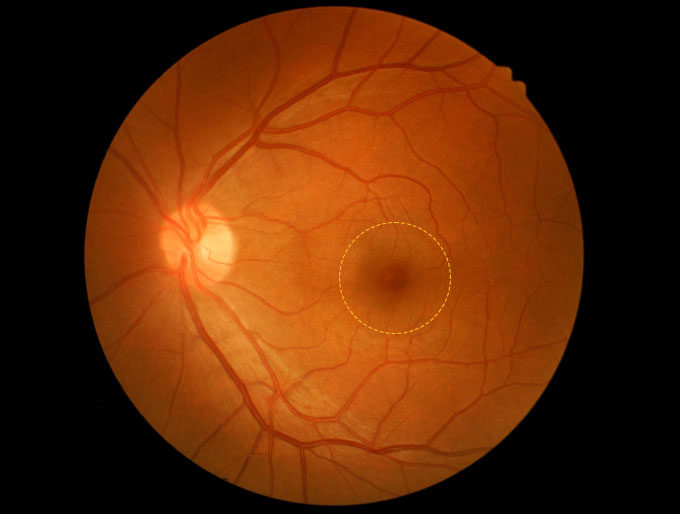
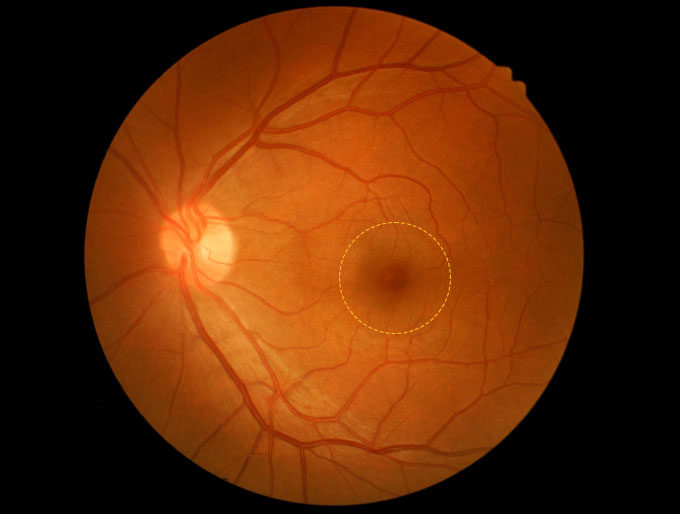
A macular hole is an actual hole or a full-thickness disorder in the macula of your eye, the central part of your retina. The retina is the part of your eye that contains nerve cells that react to light and allow us to see. A macular hole generally happens in just one eye, although it can happen in both eyes.
In the middle of the retina (the macula), the nerve cells are very close together. Sometimes, the jelly-like substance that fills your eye — the vitreous humor — changes its consistency and, as it shrinks, it can pull on the central macula and cause a macular hole to form. A macular hole can affect vision in a variety of ways, but it mainly affects your central vision (the things that you can see in the center of your vision). It affects activities like driving and reading.
How common is this condition?
One U.S. study indicates that the number of new cases of macular hole is 7.8 people per 100,000 people per year. The condition is more common among women and people assigned female at birth (AFAB). It happens much more often in people ages 55 and over, but it can happen to anyone.
Are there types of macular holes?
There are primary and secondary macular holes. A primary macular hole is one that develops without any eye injury and isn’t due to another medical condition. A secondary macular hole is a macular hole that occurs with or due to another disease or condition such as trauma or eye inflammation (uveitis).
There are a couple of ways that ophthalmologists may classify macular holes. These are called staging systems. One system uses four stages, with the first stage being the least severe and the fourth being the most severe. A newer system has three stages of macular holes based on the results of imaging tests. Your eye care provider will give you information on how severe the macular hole is.

What are the symptoms of a macular hole?
The early symptoms of a macular hole include:
- Blurred vision.
- Distorted vision. Straight lines might be curvy or wavy.
- Difficulty reading small print.
A later sign of a macular hole is a dark or blind spot in the center of your vision.
When a macular hole causes these symptoms, they’ll occur in the eye with the macular hole.
If any of these symptoms occur, it’s important to make an appointment with your eye care provider as soon as possible.
Symptoms and Causes
In most people, macular holes are due to vitreous traction that’s more likely to happen with aging. Sometimes a macular hole is the result of an injury or a medical condition that affects the eye, including being very nearsighted.
You may be more likely to develop a macular hole if you have:
- A very high degree of myopia (nearsightedness).
- Inflammation within your eye (uveitis).
- Eye trauma.
Risk factors for macular holes include:
- Aging.
- Being a woman or assigned female at birth.
- Experiencing eye trauma.
- Being very nearsighted.
- Previous eye surgeries or eye inflammation.
An untreated macular hole may lead to these complications:
- A loss of vision, especially central vision.
- A macular-hole-associated retinal detachment.
- Increased size of the macular hole.
Open-angle glaucoma
This is the most common type of glaucoma. The drainage angle (where the aqueous humor drains from the eye) is open but doesn’t function efficiently enough. This reduced drainage of aqueous humor leads to an increase in pressure inside the eye, which results in a gradual loss of peripheral vision. This can be compared to an air filter that collects dust over time and eventually becomes too clogged to function well
Angle-closure glaucoma
Angle-closure glaucoma occurs when the drainage angle is completely blocked. This type of glaucoma is often found in farsighted eyes of older individuals. It prevents fluid from draining out of the eye, leading to a sudden spike in eye pressure. This extreme pressure increase causes fluid to build up in the cornea, resulting in blurred vision, headaches, severe eye pain, and the appearance of halos around lights.
Chronic angle-closure glaucoma
In this type of glaucoma, the condition is painless and involves a more gradual closure of the drainage angle.
Secondary glaucoma
Secondary glaucoma develops when scar tissue, cells, or pigments block the drainage angle. Secondary glaucoma leads to a gradual loss of peripheral vision. Pseudoexfoliative glaucoma and pigment dispersion glaucoma are examples of secondary glaucoma. A secondary glaucoma can also develop from a hemorrhage in the anterior chamber of the eye.
Congenital glaucoma
Congenital glaucoma is a rare condition where the drainage angle is impaired or blocked from birth. To prevent blindness, this condition must be treated shortly after birth. Symptoms include enlarged eyes, a cloudy cornea, light sensitivity, and excessive tearing.

Diagnosis and Tests
How is a macular hole diagnosed?
Your eye care provider will begin by asking you about your family and medical history. You’ll want to tell them about any type of medication — prescription and over-the-counter (OTC) drugs — that you take. Your provider will then do a complete eye exam, which will include a slit lamp exam. Your provider will put eye drops in your eyes to make your pupils larger and allow for retina examination.
What tests will be done to diagnose a macular hole?
Your ophthalmologist will probably order one or more of these tests to examine your retinas:
- Optical coherence tomography.
- Fundus fluorescence angiography (also called fluorescein angiography).
- Fundus photography.
Management and Treatment

The most common treatment for macular holes is a procedure called a vitrectomy. A vitrectomy is a surgery during which a retina specialist removes the vitreous gel of your eye. Your surgeon, an ophthalmologist trained in retina surgery, may also remove any bits of tissue (membranes) that may be putting tension on your macula.
Your surgeon will put a sterile gas into your eye to keep pressure on the hole until it heals. You may have to stay in a facedown position for one to seven days to keep the bubble in place so the hole will close.
If you have a small hole, your retina specialist may suggest watching and waiting rather than treating it. Sometimes an early-stage macular hole will close on its own.
Possible complications of a vitrectomy may include:
- Retinal detachment.
- Infection.
- Glaucoma.
- Bleeding.
- The macular hole reopening or never closing.
Cataracts are expected to progress in any person who’s having retina surgery.
If you have a vitrectomy, you may need to spend up to a week with your head down to keep the gas bubble in the correct position. The gas bubble lasts three to eight weeks and your vision remains blurry while the gas bubble’s in the eye. It may take several months for your vision to improve and stabilize.
Can a macular hole be prevented?
There’s no way to prevent a macular hole. You may reduce your risk by:
- Using protective eye coverings when working or participating in contact sports.
- Having regular eye examinations. This may not prevent a macular hole, but your provider will be able to find a macular hole earlier if you follow a recommended exam schedule.
- Taking care of your eyes and managing your blood sugar levels, if you have diabetes, and your blood pressure, if you have hypertension.


Outlook / Prognosis
What can I expect if I have a macular hole?
The success rate for vitrectomy surgeries is over 90%. The surgery is most successful when the hole is smaller and more recent. You may regain most or some of your lost vision, but the amount of vision regained may vary.
When can I go back to work or school?
You’ll need to take some time away from work or school. The length of time may vary depending on the type of work you do. Ask your surgeon about what you need to do or to avoid doing after the procedure.
You probably won’t be able to drive for up to six to eight weeks, and you won’t be able to fly for about that long, too. It takes this long for your body to absorb the gas. Changes in air pressure may make the bubble in your eye get bigger and dangerously increase the pressure in the eye. Avoid any type of activity that involves changes in air pressure.
What is the outlook for a macular hole?
If you get treatment sooner, or if the hole is small, your prognosis (outlook) is good.
Without treatment, you may lose much of your central vision, but you’ll retain your peripheral (side) vision.
When should I see my healthcare provider?
Everyone should get regular eye appointments. Apart from these, see your eye care provider any time you notice a change in your vision. If you experience extreme pain, or if you have a sudden loss of vision, go to an emergency room.
What questions should I ask my healthcare provider about a macular hole?
If you have a macular hole, you may want to ask your healthcare provider:
- What type of treatment do you recommend?
- What are the side effects or complications related to this treatmen
- Will the macular hole happen again?
- How can I take care of my eyesight?
- Will I still be able to drive?
Eyes are fragile and important. Knowing that you have an eye condition like a macular hole may cause anxiety. Surgery to treat a macular hole is typically successful, and the odds are better when your provider can find the hole when it’s recent and small. That’s one reason to see your eye care provider on a regular basis.

